The NHS Workforce Plan is “achingly vague” when it comes to how the health service will retain staff and should mention the “crucial” matter of pay, according to former doctor and author Adam Kay.
Mr Kay was speaking at a one-off session of the Health and Social Care Committee, which was looking at whether the 15-year strategy actually goes far enough to tackle the challenges faced by the NHS.
He described it as “achingly vague” in detailing how the NHS plans to keep doctors practising in England.
“I see no ambition and I see no detail whatsoever,” he added. “It’s just it’s achingly vague. I don’t know what’s realistically being proposed to retain all these doctors.
“It’s all very well running the tap but the plug is very much out at the moment.”
Mr Kay also said the NHS Emeritus Doctor Scheme – an initiative to allow retired doctors to keep working – is not retention, but “resuscitation”.
He added: “Wellbeing is a huge part of it but so is pay. I think it’s borderline laughable that pay gets not a single sentence. It needs to be acknowledged as a crucial thing.”
Referencing doctors moving overseas for better wages, Mr Kay said: “If no-one’s looking after you, whether it’s in terms of wellbeing or your pay, why wouldn’t your head be turned by that?”
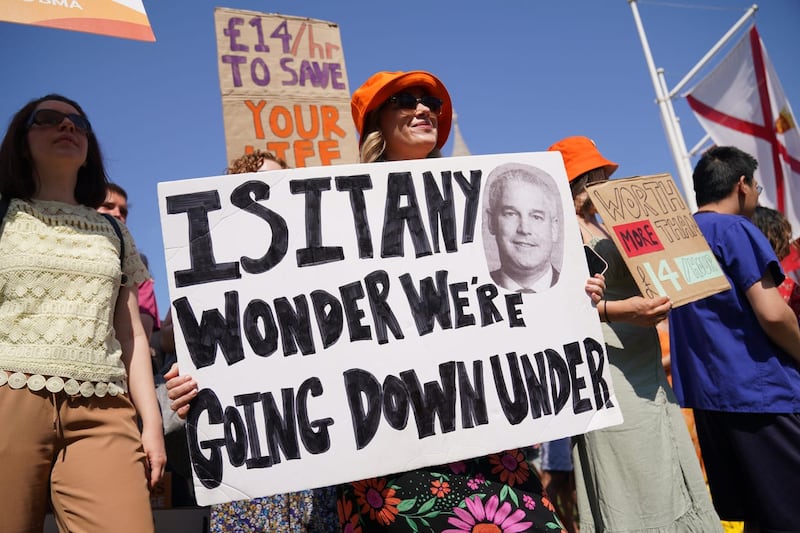
The comments come amid waves of industrial action in the NHS, with junior doctors set to walk out for five days at 7am on Thursday in an ongoing row with the Government over pay.
They will be followed by consultants, who are striking for two days from July 20, and radiographers, who will walk out for two days on July 25.
Prof Kamila Hawthorne, chairwoman of the Royal College of General Practitioners Council, was also a witness and said there is more to retention than money.
“What we need to do is to make life for doctors so good that they don’t want to leave. That’s what we should be doing, rather than punishing the ones who leave.
“It really is not about money, it’s about valuing people, and it’s about not giving them a workload that is so unbearable. Certainly general practice is very difficult to work more than three full days a week, because you’re putting in way more than you should.”
The long-awaited NHS Workforce Plan was unveiled by the Government last month, promising to hire 300,000 additional workers over the next 15 years.
As well as recruitment and retention, training also forms a large chunk of the blueprint.
There are aims to double medical school training places to 15,000 by 2031, increase the number of GP training places to 6,000 and double the number of adult nurse training places.
Apprenticeships will also be ramped up. It is estimated that 16% of all training for clinical staff, including doctors, nurses and other health professionals, will be offered through degree apprenticeships by 2028, including 850 doctor apprenticeships.
However, Patricia Marquis, England director at the Royal College of Nursing (RCN), told the committee that a significant hike of apprentices in the nursing pipeline is a “real, real worry”.
She said the way she trained “was in a way an apprenticeship”, adding: “I can speak from personal experience about being put in positions where I was doing things way outside of the scope of what I should have been doing with the amount of education and supervision that I had.
“So it varies because this is different. It is an apprenticeship, it’s delivered in a different way. But the risk of people going beyond the scope of what they are supposed to be doing at a particular point of training, especially given the pressures they’ve got, really increase. And when we’re talking about such a significant increase in the number of apprenticeships within the nursing pipeline, that becomes a real, real worry for us.”
General Medical Council (GMC) chief executive Charley Massey said he “welcomes the ambition” of the plan but said the training capacity should be in place to deliver that ambition.
Prof Hawthorne also pointed out it will be a “good 10 to 15 years” before the sector sees new GPs coming through from medical school.
“There is nothing at the moment that would stop a GP from wanting to leave other than hope on the horizon,” she added.








