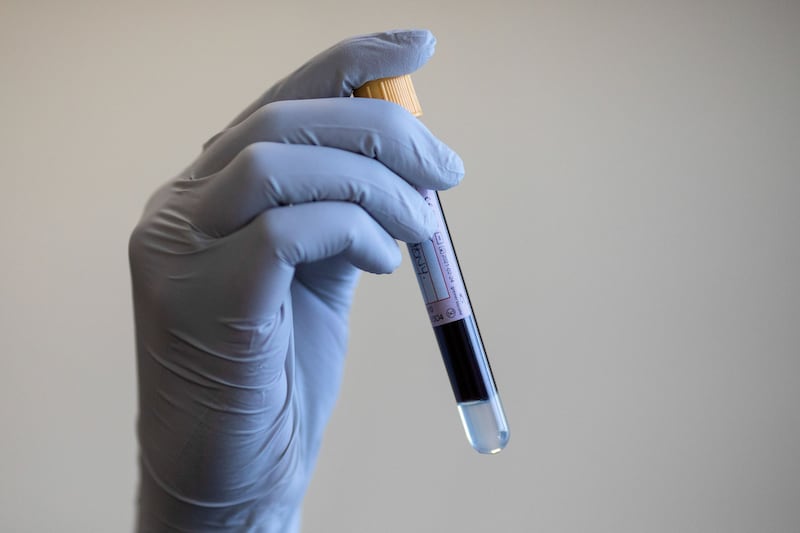
A blood test that can detect Parkinson’s disease could be a step towards finding a cure for the condition, researchers have suggested.
It is hoped the findings of a US study, published in the journal Science Translational Medicine, could lead to treatments that halt the progression of the disease before it affects a patient’s nervous system, or even help reverse damage on a cellular level.
Laurie Sanders, an associate professor in Duke School of Medicine’s departments of Neurology and Pathology, said: “Currently, Parkinson’s disease is diagnosed largely based on clinical symptoms after significant neurological damage has already occurred.
“A simple blood test would allow us to diagnose the disease earlier and start therapies sooner.
“Additionally, a clear-cut diagnosis would accurately identify patients who could participate in drug studies, leading to the development of better treatments and potentially even cures.”
A team led by Prof Sanders comprising neuroscientists from Duke Health developed the blood test by examining DNA damage in the mitochondria – small, energy-producing structures found in the cell.
Mitochondria contain their own DNA that can be damaged separately from the nuclear DNA that makes up most of a human genome.
The team developed an assay which showed higher levels of mitochondrial DNA damage in blood cells collected from patients with Parkinson’s disease compared to people without the condition.
The test also identified high levels of damaged DNA in blood samples from those with the genetic mutation LRRK2, which has been associated with an increased risk of Parkinson’s.
The team analysed cells further to explore whether their test could determine the effectiveness of a therapy that targets the LRRK2 mutation.
Prof Sanders added: “Our hope is that this assay could not only diagnose Parkinson’s disease, but also identify drugs that reverse or halt mitochondrial DNA damage and the disease process.
“This disease takes a terrible toll on people, and we are still just treating the symptoms. It’s important to get new, effective treatments over the finish line.”