COUNSELLING should be available in every GP practice in Northern Ireland, the group behind a mental health campaign has said.
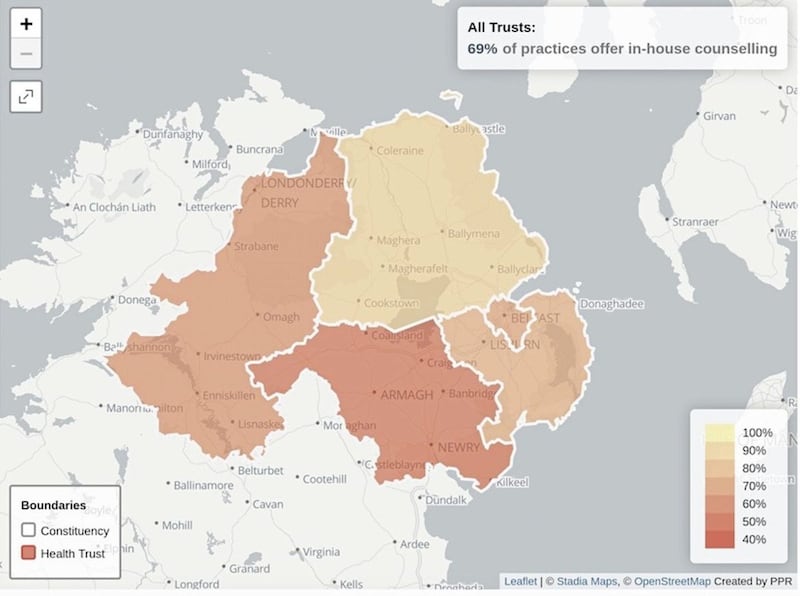
Research by Participation and the Practice of Rights (PPR) has found there are huge disparities in the availability of counselling provided by GP practices across the north's five health trusts.
While around 89 per cent of practices in the Northern Trust have an in-house counsellor, only 51 per cent do in the Southern Trust.
There are also clear differences at a constituency level.
[ READ MORE: Curious about giving remote therapy or counselling a go?Opens in new window ]
The figures show that all GP practices in East Antrim have in-house counselling, compared to only 40 per cent in West Tyrone, 45 per cent in South Down, 50 per cent in West Belfast and 57 per cent in Newry and Armagh.
PPR said GP practices have reported a significant increase mental health queries as a result of the pandemic.
The group's #123GP campaign has called on health minister Robin Swann to ensure that GP practices are given enough resources to offer counselling to anyone who needs it.
Campaigners said that no one should wait longer than two days for an urgent appointment and 28 days for a routine one.
The group said people should also be given the option to have counselling either via their GP practice or through talking therapy hubs run by the health trusts.
Sara Boyce, Mental Health Campaign Organiser at PPR, said the pandemic will continue to have an effect on mental health.
"GPs will have a key role in connecting people to the support they need, so it’s vital that they are properly equipped to do this," she said.
"Counselling is one effective treatment but at this present time accessing counselling through your GP practice is a post-code lottery. In some areas every GP practice offers this service but in others, less than half of GP practices can offer it.
"This cannot be fair or right.
"Now is the time, with the development of a ten-year Mental Health strategy, for the Minister for Health to ensure that all GP practices are resourced to provide timely access to counselling.
"Let’s ensure that everybody can get the help they need, regardless of where they live."







