EXPERT virologists embarking on a major study to discover drugs that will treat the "sickest" Covid-19 patients cannot begin their search until they receive specialist protective masks and clothing.
The Irish News has learned that academics at Queen's University Belfast (QUB) have been hit by supply shortages of Personal Protective Equipment (PPE) - as well as frontline hospital staff and care home workers.
Last week it emerged the small team of virologists had received a £300,000 share of a £20 million grant the British government had set aside for vital research into anti-viral drugs.
Virologist Dr Linday Broadbent revealed they are desperate to begin work by testing multiple drugs on 'mini human lungs' grown in their Belfast laboratory - but said this cannot begin until they "receive the virus".
Read More: Nurses express fears about dire PPE shortage for staff treating suspected Covid patients
"The grant starts this week. We've been getting all the health and safety in place but we're having issues sourcing PPE. This issue don't just affect hospitals and other frontline staff. It's also affecting research because we cannot work with the virus unless we have the proper protective clothing.
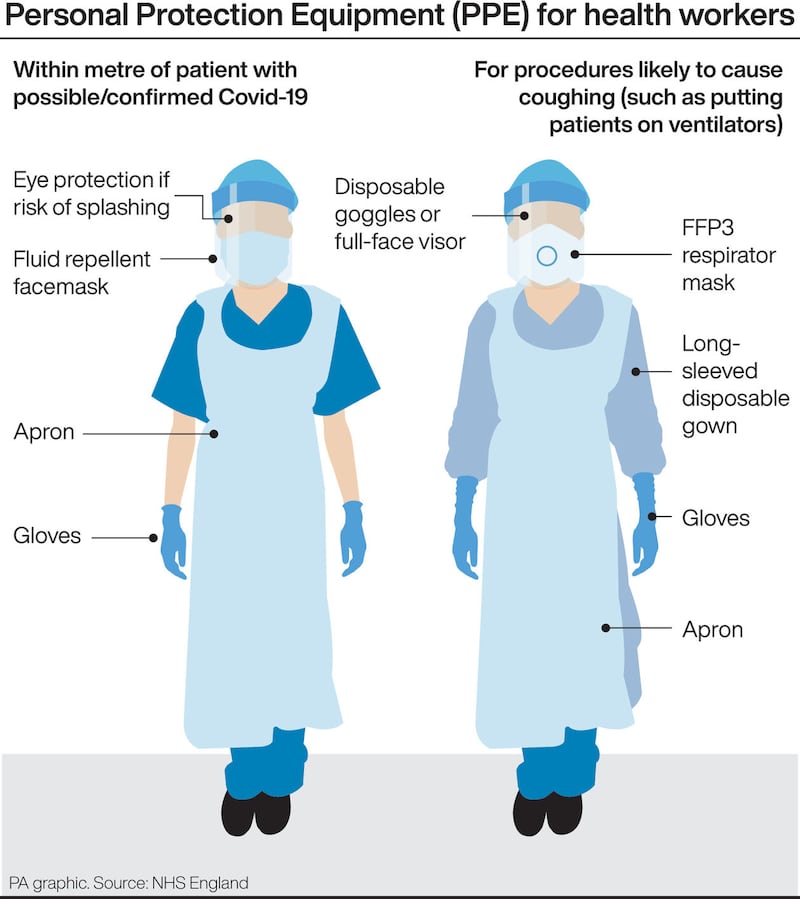
"Health officials will not give us the virus until they're sure the facilities are safe and we are safe."
Dr Broadbent explained how they grow cells from human lungs - complete with mucus and small hairs - which work "fantastically well" as they replicate how a person will respond.
"Our grant is to look for treatments. So we have this massive library of drugs that are already FDA approved. We're going to test about 1000 drugs very rapidly and figure out if any of those have an effect on the virus and reduce the viral growth," she said.
"Once we have narrowed it down to a few drugs we have this cell culture system - I like to call them 'mini-lungs' - because they produce mucus. Because they're actual cells from humans, they respond the way people would.
"The drawback is that people respond differently so we need to try several different cells from several different people."
The team's lead is Ultan Power, a Professor of Molecular Virology at the Wellcome-Wolfson Institute for Experimental Medicine at Queen's.
The expert researchers are currently studying literature around the "best candidate" drugs and trying to narrow down those already licensed so they don't have to go through safety tests.
"It takes two months for lung cells to be ready to use, so within that time we hope to have the results from the initial drug screening. We infect those cells, we put the drugs on top and then we'll look to see if the cells are dying or are the cells are surviving in the presence of the drug. We're looking for increased cell survival with the treatment of the drug," Dr Broadbent added.
The virologists will also examine different levels of dosing and test for how long after infection the drugs still work.
"When a person gets incredibly sick they'll already have been infected for several days so there's no point finding a drug that works if we have to give it to them on day one. We have to find a drug that works when a person is at their sickest. We want to infect our mini-lung cultures, leave it for a few days, and then put a drug on and see if we can still help ourselves to survive," she added.
International studies have examined some anti-HIV and anti-Ebola drugs while US President Donald Trump yesterday tweeted about an anti-malaria drug, hydroxychloroquine, being among the 'biggest game changers in the history of medicine" for its potential effects against Covid-19.
However, the European Medicine Agency said the efficacy of hydroxychloroquine had not been proven in relation to coronavirus treatment.
Dr Broadbent said they were keeping an open mind on all drugs.
"We're not just looking at anti-viral drugs. We're looking at drugs that can be used for inflammation, heart disease. We're not narrowing it down just to anti-virals because I think we might miss something that could work," she added.
As the global number of Covid-19 related deaths reached more than 40,000 last night and Ireland prepares for a surge in cases and fatalities over the next fortnight, Dr Broadbent said timing was crucial in discovering new treatments.
"We're only funded for a year and that's to have absolutely everything done and out the door. So I would like to have the results of the high throughput screening - our initial testing of the 1000 drugs - done within six weeks or two months. But that is dependent on us getting the PPE," she said.








