‘FAMILY’ is the term that keeps popping up when staff, past and present, speak about the Mater Hospital.
Founded by the Sisters of Mercy in 1883, the north Belfast facility was known for its strong Catholic ethos but its central aim was to “care for the poor of the city” regardless of creed – and was the first to treat injured British soldiers during he Troubles in 1969.
From its humble beginnings, the ‘community’ hospital would become renowned for its excellence in the treatment of pancreatic and liver cancers, housing a regional surgical unit.
Close-knit teams of surgeons, theatre nurses, ICU nurses, anaesthetists and support staff worked hand in glove across this and multiple other medical specialties while its maternity unit also remained first choice for many expectant mothers.
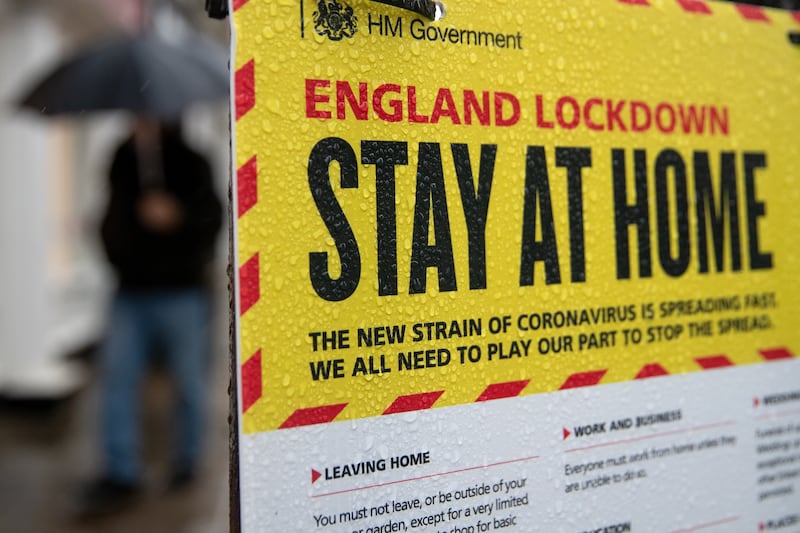
On March 23 last year, the Belfast trust announced it had designated ‘the Mater’ as its Covid-19 hospital.
By noon the following day, “all respiratory ambulance admissions” were diverted to the Crumlin Road site while staff from other trusts were redeployed in preparation for the first surge.
Walk-ins could no longer go to the Mater’s A&E department.
For A&E consultant Dr Eoghan Ferrie and respiratory nurse consultant Anne Marie Marley, the “unique” closeness of staff has been key in surviving the unprecedented pressures since then.
“I did a fair bit of my training in the Mater and I know totally the ‘family feel’ to that site,” Dr Ferrie said.
“It’s always maintained that and it is one of the real strengths of it – and is why the hospital has managed to get through what it has in the last 18 months.
“There is no doubt that some of the outcomes from Belfast in terms of the critical care support and enhanced respiratory support are far superior to what we are seeing even against peers across the UK.
“A lot of that is down to the experience and just camaraderie that goes on at that site.”
With a surge in coronavirus hospital admissions across Northern Ireland over the past six weeks, Ms Marley said staff are trying their “absolute damnedest” in what is an “extremely busy” period.
The hospital no longer has an ICU, with those requiring ventilation moved to the City Hospital.
“There were 163 patients in beds in the Mater today, with only one empty bed this morning. We are full to capacity,” the senior nurse told The Irish News last Wednesday.
“Our Covid positive patients will be on enhanced respiratory support but not all will require this. We have your awake, sick patients. We try and cohort them here on this site.
“But we’re beginning to have patients who have made finally it out ICU and are coming back to us for intensive rehabilitation. The hospital is extremely busy.
“Everybody is working so collectively hard to do the right thing and are so mindful of minimising risks.
“The pandemic has changed and the patients have changed – we are constantly having to flex and change and people are having to move.”
No operations are currently performed in the Mater. Its hepatobiliary surgery – which treats the pancreas, liver and bile ducts – transferred to Belfast City Hospital last year where it is likely to continue for the “foreseeable future”, according to the trust.
Babies are also no longer being delivered at the hospital – though outpatient appointments for antenatal care and other specialties including cardiology are continuing.
A fortnight ago The Irish News asked the Belfast trust to comment on concerns about whether services would return to the Mater, in particular its hepatobiliary surgery.
The trust responded by saying that the “function and situation” of all its sites “remained under constant review” and that hepatobiliary surgery would continue at the City hospital for the “foreseeable future”.
For Dr Ferrie, the lack of assurances about what lies ahead are “unsettling”.
“I suppose one of the things colleagues in the Mater and indeed the general public want is reassurance about the future. We’re not really in a position to give that at the moment,” he said.
“We are literally working day to day and week to week. No-one is more fed up with Covid than the healthcare professionals.
“I would love to wake up tomorrow and it’s been a dream and everything is back to the way it was.
“It’s still too early to predict when surgery and critical care services are going to get integrated back in – obviously the intention is we would try to restore things back to the services that were once there.
“But at the moment there is still uncertainty, and the uncertainty unsettles me as much as it does the colleagues who want a bit more reassurance.”
As one of the leading consultants in emergency care, Dr Ferrie said the decision to change the admissions criteria for the Mater’s A&E was not just linked to the pandemic.
Prior to the outbreak, a major health service reform report recommended an overhaul of the existing A&E system, which has been plagued by severe pressures for over a decade.
“In the throes of the pandemic the DoH [Department of Health] asked us to implement some of the outworkings of the ‘No More Silos’ review, including the creation of a new urgent care centre. Something had to be done,” added Dr Ferrie.
“For now the ED at the Mater is still functioning very much as a ED. It’s still part of the integrated emergency care response for Belfast.
“Most of the patients brought here are mainly respiratory and medical ambulance patients. There are also referrals from GPs and the urgent care centre. Trauma goes to RVH.
“But it’s very hard to give absolute predictions about how things are going to develop because we don’t know how long the pandemic is going to be with us and we also don’t know what direction No More Silos work is going to take us either.”
As they prepare for winter pressures, the two health professionals urged unvaccinated people to get their jabs and called for the introduction of vaccine passports to gain entry to indoor pubs and restaurants.
“I think we should absolutely introduce the Covid passports similar to the Republic. I was on holiday down south and it made me feel more secure and didn’t impinge on me,” Ms Marley said.
Dr Ferrie also supported Covid certs as proof of entry to indoor hospitality and expressed concerns “more consideration couldn’t have been given to the issue” as the north’s vaccine uptake rates lag significantly behind the south.
While political pressure began mounting last week for vaccine passports, they were rolled out in the Republic at the end of July.
Dr Ferrie added: “I know some people personally who have reasons not to take the vaccine.
“I think part of it is a failure to understand the purpose of vaccination programmes – they are public health programmes, it’s just not to protect individuals from getting sick but to protect populations.
“If it’s just about people being happy to gamble as an individual on getting sick or not – and if you get enough people with that opinion – it affects population.
“The same people can’t then turn round and complain about long waiting lists and not being able to get surgery. Their behaviour is allowing the health service to be overwhelmed.
“I worked in Australia for a year, who are behind us with the vaccination rollout.
“One of the colleagues who I keep in touch with made an interesting comment saying that in the movies, the film ends when the vaccine comes and everybody is cheering. That’s not what’s happening in real life.”
Almost 88 per cent of the north’s adult population have received their first dose but a quarter of 18-29-year-olds have not been jabbed.
Ms Marley said they had noticed more younger people with no underlying illnesses or ‘comorbidities’ requiring hospital beds after contracting the virus.
She also appealed to pregnant women to get jabbed and described the levels of illnesses they had seen among some expectant mothers as “horrendous”, especially among those forced to remain in hospital while their baby is sent home.
“You can just imagine how distressing it is on the wards for young nurses caring for very sick pregnant women coming in during their third trimester. That is something we have never had to witness,” the senior nurse said.
“That stays with the nurse, the consultants.”
As a workforce appeal for recently retired healthcare professionals gets underway, staff shortages and the burnout felt across the entire health service workforce remains a central concern going into the busy winter period.
Hospital admissions – which spiked over a month ago and led to public appeals for people not to attend A&E unit – are starting to come down slowly.
Dr Ferrie added: “As an organisation we’re preparing for the worst and hoping for the best.
“There is a lot of concern – we’re not at great starting point. The less staff you have the more you ask of the staff who are there. People are already tired. People need their breaks. And that goes back to us being able to support them.”
Nursing in particular has been badly hit, with a heavy reliance on agency and bank staff.
While some overseas nurses are due to take up posts at the north Belfast hospital, they will require training and mentoring.
“We’re doing our best to have the right, safe number of beds open where patients can be looked after,” added Ms Marley.
“Another challenge is that teams on wards are trying to look after relatives at home and keep them informed. It adds extra layer.
“We have learned a lot over the last 18 months and I suppose if there had to be a designated hospital it is a good thing it is the Mater. It is perfectly sited to be looking after patients and each other.
“But we are literally longing for the day when we get back to functioning any way like we used to function and keep everything that is the essence of the Mater and the quality of the delivery patients are used to.
“Our job for now is to keep our staff’s heads up and pull on whatever resilience they have to keep going.”