Healthy gut bacteria improves the success of cancer treatment, a new study suggests.
Researchers say the findings are a key step forward in the fight against multiple types of cancer including melanoma, the most deadly form of skin cancer.
As less than 50% of people respond positively to immunotherapy for melanoma, finding ways to improve this number is crucial, the scientists suggest.
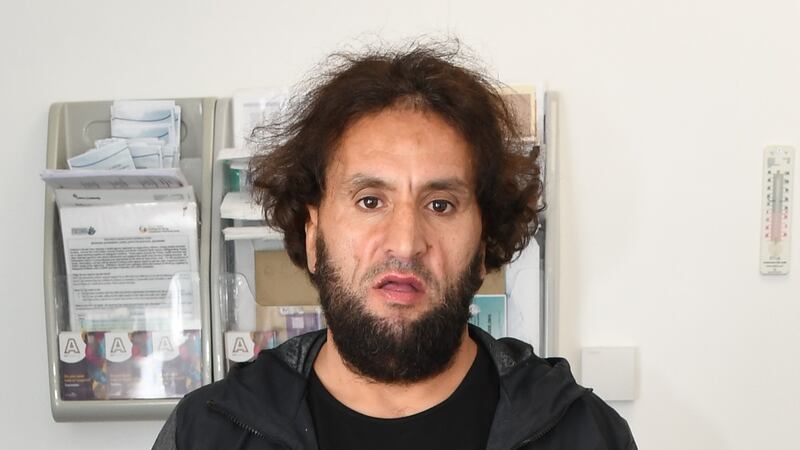
The study found that melanoma patients who receive therapy to help their immune system kill cancer cells respond differently to treatment depending on the types of microbes in their gut.
The new research suggests the microorganisms that hinder therapy have more of an influence than ones that are beneficial.
Dr Karla Lee, clinical researcher at King’s College London and first author of the study, said: “Preliminary studies on a limited number of patients have suggested that the gut microbiome, as an immune system regulator, plays a role in the response of each patient to cancer immunotherapy, and particularly in the case of melanoma.
“This new study could have a major impact on oncology and medicine in general.”
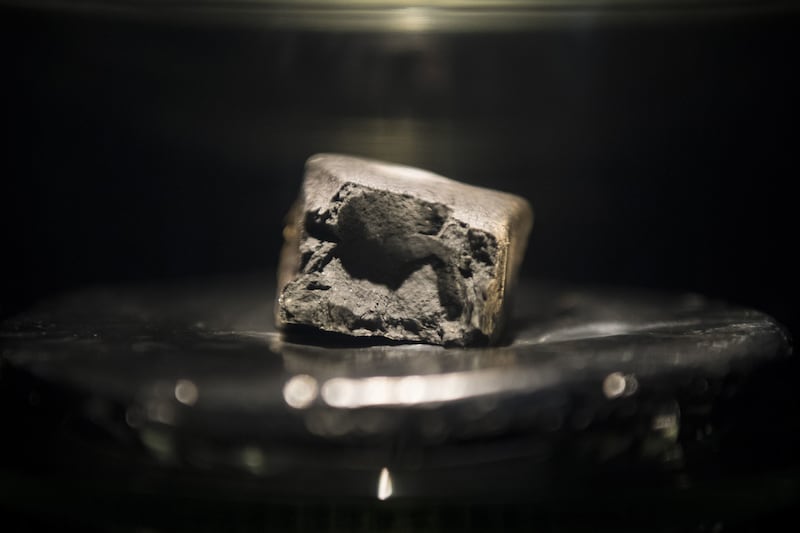
The microbiome, the set of microorganisms that live in the intestines, can be altered through dietary changes, probiotics and faecal transplantation.
Researchers suggest understanding the characteristics of the microbiome could allow doctors to change a patient’s microbiome before starting treatment.
Co-author Professor Tim Spector from King’s College London said: “This study shows the chances of survival based on healthy microbes nearly doubled between subgroups.
“The ultimate goal is to identify which specific features of the microbiome are directly influencing the clinical benefits of immunotherapy to exploit these features in new personalised approaches to support cancer immunotherapy.
“But in the meantime, this study highlights the potential impact of good diet and gut health on chances of survival in patients undergoing immunotherapy.”
The study put together the largest group of patients with melanoma and samples of their gut microbiome from five clinical centres in the UK, the Netherlands and Spain.
Researchers carried out a large-scale sequencing of the gut microbiome to investigate whether there was a link between the make up of the gut microbiome and response to immunotherapy.
They found a complex association that involves different bacterial species in different patient groups.
The presence of three types of bacteria appeared to be associated with a better immune response.
The research also found that the microbiome itself is strongly influenced by factors including the make-up of the patient’s body and diet.
Co-author Professor Nicola Segata from the University of Trento, Italy, said: “Our study shows that studying the microbiome is important to improve and personalise immunotherapy treatments for melanoma.
“However, it also suggests that because of the person-to-person variability of the gut microbiome, even larger studies must be carried out to understand the specific gut microbial features that are more likely to lead to a positive response to immunotherapy.”
The study is published in Nature Medicine and co-ordinated by King’s College London, CIBIO Department of the University of Trento and European Institute of Oncology in Italy, University of Groningen in the Netherlands and funded by the Seerave Foundation.
Dr Simon Vincent, director of research, support and influencing at Breast Cancer Now, said: “A healthy gut microbiota is important in regulating the body’s response to disease, however antibiotics can disrupt the balance of bacteria in the gut.
“Whilst links between antibiotics and different types of cancer are being discovered, more work is needed to understand the complex relationship.”
He added: “Last year, Breast Cancer Now funded researchers at the University of East Anglia found a possible link between antibiotics and the speed of breast cancer growth.
“Whilst this may sound alarming, this was early stage research tested in mice.
“Excitingly, our research provided a crucial insight that by targeting a specific immune cell called ‘mast cells’, we could counteract the potential negative effects of antibiotics and halt antibiotic-induced breast cancer growth.
“We must now further investigate the effect of antibiotics in breast cancer treatment so that we can find the best way to stop tumours from growing.”