Personalised vaccines, when given in combination with a drug that boosts the body’s natural defences to fight cancer, has shown “promising signs” in early clinical trials of patients with advanced cancers.
Researchers have found the experimental treatment, which involved administering tailor-made vaccines alongside immunotherapy drug atezolizumab, was “well tolerated” and the participants experienced “low-to-moderate” side effects.
The findings from the phase one clinical trial, which was designed to test the safety of the treatment, were presented in the AACR Virtual Annual Meeting II, a scientific conference running from June 22-25.
The researchers are now looking to expand their investigation to understand more about the potential benefits of personalised vaccines for patients with earlier-stage cancers.
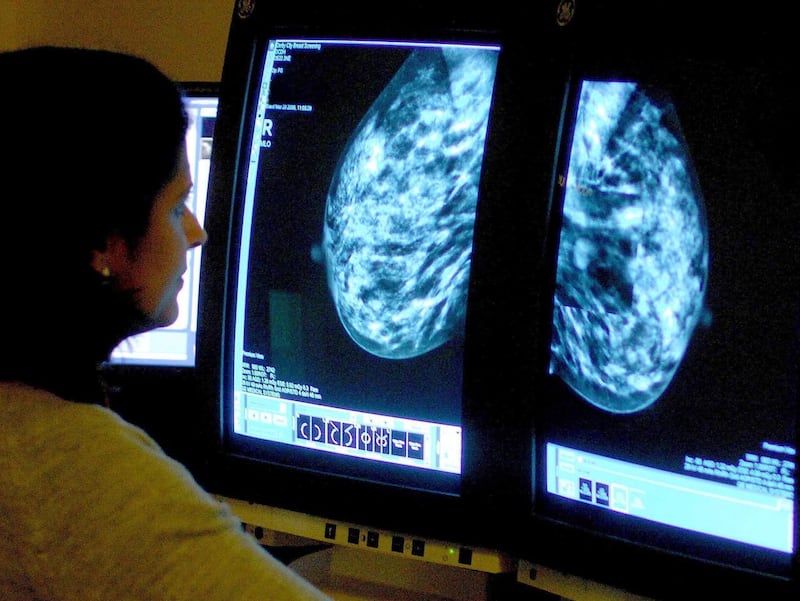
An international team of scientists, led by clinicians in the UK, investigated the effects of personalised vaccines in 144 patients who had different types of advanced cancers, including lung, breast and bowel.
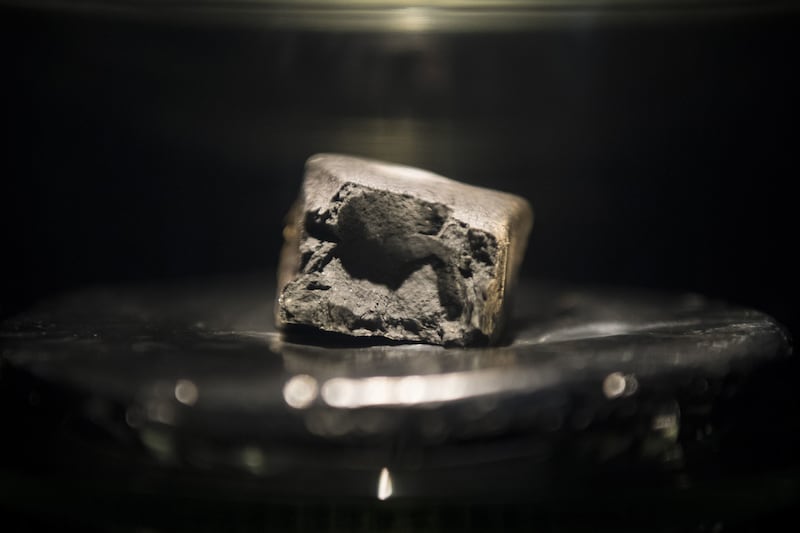
To develop the vaccine, the scientists first took a biopsy of a patients tumour and used artificial intelligence to identify a group of proteins known as neoantigens, which are produced in tumour cells and have not been previously recognised by the immune system.
Using this information, they were able to design a type of cancer vaccine known as messenger RNA vaccine, which can be tailored to target the “unique differences” in tumours of every cancer patient.
Dr Juanita Lopez, a consultant medical oncologist at The Royal Marsden NHS Foundation Trust and The Institute of Cancer Research, London, who led the trial, said: “Many cancers are able to successfully avoid the immune system, and we are only starting to understand the myriad ways in which cancers can do this.
“Because many mutations are not shared between cancers, a personalised treatment approach that targets individual tumour neoantigens may be a viable immunotherapeutic strategy for numerous patients with cancer.”
During the induction phase of the trial, patients received one of the different doses of the vaccines, ranging from 15 to 50 micrograms once per week, for six weeks.
The seventh and eighth doses were administered fortnightly, while atezolizumab was given on a 21-day cycle.
Patients received a booster dose of the vaccine during the seventh cycle of atezolizumab, along with a maintenance dose of the vaccine every 24 weeks following the induction phase.
The personalised treatment was well tolerated, with patients largely experiencing low-to-moderate side effects, the researchers said.
But only 8% of patients saw a reduction in their tumours and 49% had stable disease, where their tumours were neither growing nor shrinking.
According to Dr Lopez, this low clinical response rate is “likely because many of the patients treated in our study had very advanced disease, and were heavily pre-treated”.
However, analysed blood samples from 63 patients showed that the immune system had been activated in 73% of them, which the researchers believe is a response to the personalised vaccine treatment.
But they add further studies with a larger patient population are needed to understand more about the benefits of this treatment.