Antibiotic-resistant strains of a potentially deadly gut bacteria are spreading through European hospitals, a study suggests.
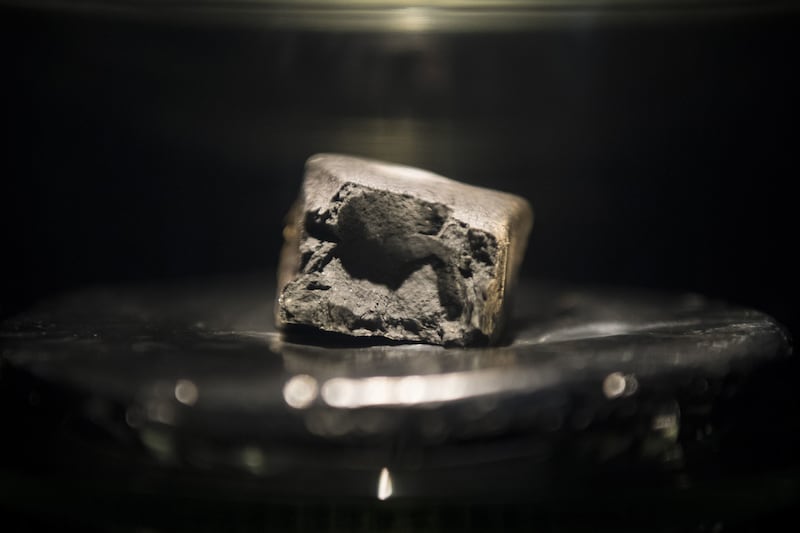
Klebsiella pneumoniae are resistant to the carbapenem antibiotics that represent the last line of defence in treating infections, and are therefore regarded as extremely drug resistant (XDR).
The bacteria normally live in human intestines, where they are harmless. But if they spread to another part of the body, they can cause severe infections.
It is estimated that 341 deaths in Europe were caused by carbapenem-resistant K. pneumoniae in 2007. By 2015 the number had increased six-fold to 2,094.
Researchers say the high number of deaths is down to the fact that once carbapenems are no longer effective against antibiotic-resistant bacteria, there are few other treatment options left.
Young children, the elderly and immuno-compromised individuals are particularly at risk.
A Europe-wide survey of the Enterobacteriaceae family of bacteria was conducted by researchers at the Centre for Genomic Pathogen Surveillance, based at the Wellcome Sanger Institute at the University of Freiburg, and their partners.
Scientists found that hospitals were the key facilitator of the bacteria spreading, with more than half of the samples carrying a carbapenemase gene closely related to others collected from the same hospital and a similarity in samples within individual countries.
The results, published in Nature Microbiology, will inform public health efforts to control the spread of these infections in hospitals across Europe.
Researchers say the survey is the largest of its kind and is the first step towards consistent surveillance of carbapenem-resistant bacteria in Europe.
More than 2,000 samples were collected from patients across 244 hospitals in 32 countries, including the UK, and sent to the Wellcome Sanger Institute, where the genomes of 1,700 of them were sequenced.
Scientists identified a small number of genes that can cause resistance to carbapenem antibiotics when expressed.
When the information stored in DNA is converted into instructions for making proteins or other molecules, it is called gene expression. These genes produce enzymes called carbapenemases, which “chew up” the antibiotics, rendering them useless.
According to the researchers, the major concern to public health is the recent emergence of a small number of “high-risk” clones carrying one or more carbapenemase genes, which have spread rapidly.
It is thought the heavy use of antibiotics in hospitals favours the spread of these highly-resistant bacteria.
Dr Sophia David, first author of the study, based at the Centre for Genomic Pathogen Surveillance, said: “The ‘One Health’ approach to antibiotic resistance focuses on the spread of pathogens through humans, animals and the environment, including hospitals.
“But in the case of carbapenem-resistant Klebsiella pneumoniae, our findings imply hospitals are the key facilitator of transmission – over half of the samples carrying a carbapenemase gene were closely related to others collected from the same hospital, suggesting that the bacteria are spreading from person-to-person primarily within hospitals.”
Researchers found antibiotic-resistant bacteria samples were also much more likely to be closely related to samples from a different hospital in the same country, rather than across countries.
They said this suggests national healthcare systems as a whole play an important role in the spread of these antibiotic-resistant bacteria.
More effective infection control in hospitals, including looking at how patients move between hospitals, and hygiene intervention will have an impact, they added.
Professor Hajo Grundmann, co-lead author, said: “We are optimistic that with good hospital hygiene, which includes early identification and isolation of patients carrying these bacteria, we can not only delay the spread of these pathogens, but also successfully control them.
“This research emphasises the importance of infection control and ongoing genomic surveillance of antibiotic-resistant bacteria to ensure we detect new resistant strains early and act to combat the spread of antibiotic resistance.”
A second survey of the Enterobacteriaceae bacteria family across hospitals in Europe is being planned.