Q: COULD you please tell me what can help to stop hair falling out? Is it caused by a lack of vitamins and minerals?
Mrs DH
A: This is a very common complaint, and I imagine many other readers will be affected and interested in your question.
Hair loss is linked to a wide range of medical problems, generally affecting the hair growth cycle or the hair follicle itself.
The scalp has between 100,000 and 150,000 hair follicles and there are two types, terminal and vellus. Terminal hair follicles are larger, extend more deeply into the skin and, at birth, are found only on the scalp, eyelashes, and eyebrows (we develop more later in life, in areas including under the arms and the pubic region). The hairs produced are 0.06 mm in diameter or larger. Vellus follicles, found all over the rest of the body, produce shorter, finer strands, less than 0.03 mm in diameter.
All hair follicles go through cycles of growth (called anagen), periods of change (catagen) and periods of rest (telogen), where the hair is lost and falls out – growth then starts again.
At any one time, 90 per cent of the follicles on the scalp are in an anagen phase, which lasts between two and six years. By contrast, the resting phase usually lasts about three months before the hair is shed – we lose 50 to 150 hairs each day.
Hair loss may be due to abnormality of this cycle, inflammatory conditions of the follicles, or inherited abnormalities of the hair shaft (which means that strands break).
Space does not permit me to cover the entire spectrum of causes, so I will focus on female-pattern hair loss, the most common type in women, where the hair on the crown and at the front of the scalp becomes thin. Although this can happen at any time, it is most common after the menopause, and affects an estimated 70 per cent of women over the age of 70.
The thinning occurs as most of the terminal hair in the frontal area (from the hairline at the forehead going back 5cm to 8cm) and the crown changes to the vellus type.
Simultaneously, the growth phase shortens from years to months. The reason for this is not well understood, but the influence of hormones on the follicles is certainly involved.
In answer to your question, there is no evidence that vitamin or mineral deficiency is the cause. However, I always recommend that my patients with this problem consider taking Florisene, a capsule containing a form of iron and the amino acid lysine, for which no prescription is needed. There is evidence that low iron levels can be associated with hair loss, so taking this may help (the lysine improves the absorption of the iron).
With prescribed medication, the strongest evidence is for minoxidil, available as a 2 per cent solution or a 5 per cent foam. This is applied to the scalp once or twice daily and it may take four months to see results. At first, there may be excess hair loss as follicles transition from the telogen to the anagen phase, but this is not a reason to stop treatment.
Q: AS AN 81-year-old with an enlarged prostate; how do I ascertain which of the many new surgical treatments I read about is best for me?
MH
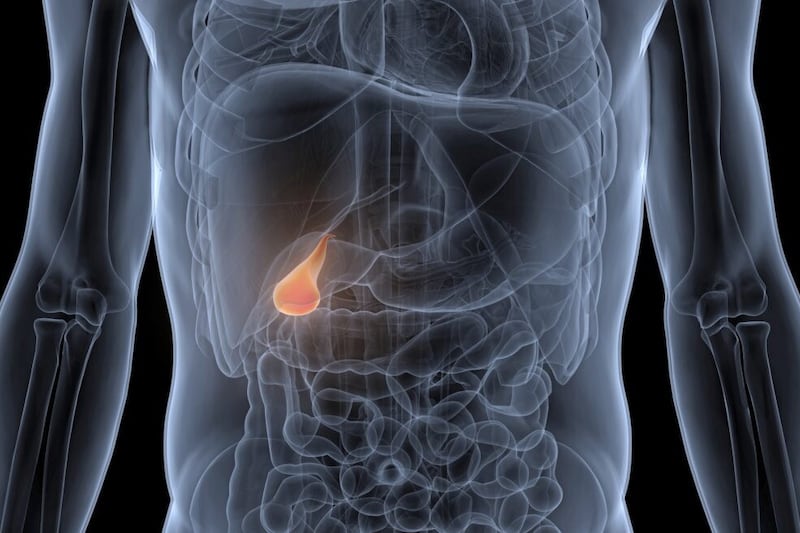
A: The prostate gland sits around the urethra, the drainage channel from the bladder. It enlarges with age – a condition called benign prostatic hyperplasia (BPH) – causing poor stream, increased frequency, urgency and the need to use the loo more than once at night.
Up to 90 per cent of men in your age group will have at least some of these symptoms.
Treatment with medication, long term, is usually the first option, but some patients experience side-effects, including headaches, dizziness and dry ejaculation. If that is the case, a surgical procedure is advised.
The standard is keyhole surgery via the urethra to remove much of the prostate tissue. But, as you are aware, there are now many other options, including Aquablation, UroLift, iTind, PAE and Rezum.
Some involve removal of prostate tissue by laser, steam energy, ultrasound or by blocking off the blood supply so the tissue shrivels.
My view is that the correct operation must be decided by your urologist, as the decision very much depends upon your precise situation, including your wish to maintain normal sexual function.
© Solo dmg media